
What is it?
Growing up – especially in a Māori or Pacific home – you may have heard the term “gout” almost always followed up by the word “attack”. Usually it’s after the big pot of raw fish or the massive tray of mussels has been demolished, and the consequences start to kick in for those prone to these attacks.
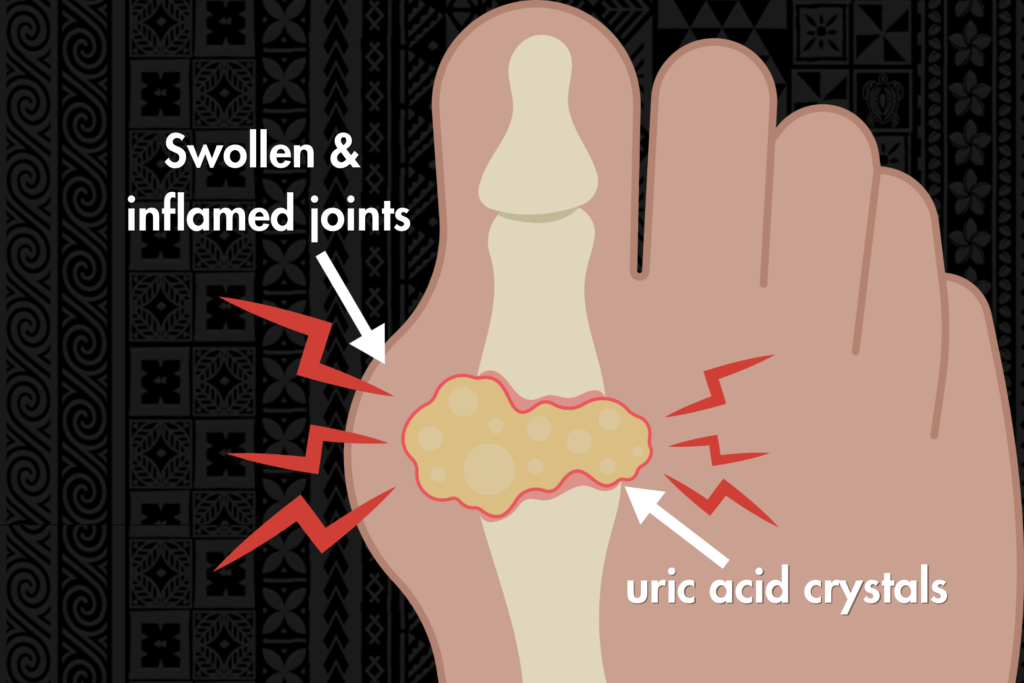
To explain it simply, gout is a form of arthritis. It forms as a result of the body having high levels of uric acid, which causes severe pain in the joints of the person who has it. There also is the possibility of potential damage to these areas of the body, which is why this condition is very serious.
This life-long condition not only reduced life expectancy, but it can also affect quality of life. Due to the severe pain it causes, it can stop people from being able to perform work tasks, care for their families, fulfil church responsibilities, or just simply enjoy life.
What causes it?
Everyone has uric acid in their bodies – in fact, our bodies actually need it. The majority of people get rid of excess uric acid by passing it through their urine.
When our bodies have a high level of uric acid, crystals start to form in the joints, causing inflammation and severe pain in these areas.
Several factors contribute to its development, including kidney disease, genetics, and diet.
Kidney disease can impair the body’s ability to get rid of uric acid efficiently, leading to its buildup in the bloodstream.
Genetics play a crucial role as well. Biological factors that some individuals inherit make them more prone to producing higher levels of uric acid, or have a reduced ability to eliminate it from their bodies.
Additionally, diet plays a significant role in triggering gout, particularly foods high in purines, such as red meat, seafood, and alcohol, which can elevate uric acid levels.
Understanding all these factors is essential in managing and preventing gout, as lifestyle modifications and medical interventions can help manage and reduce its impact on individuals’ health.
How is it diagnosed?
If you aren’t sure whether you’ve got gout, visit your doctor who will do one (or more) of the following:
- Examination: your doctor will take a look at the affected joints in your body that are in pain, and can usually conclude whether a blood test needs to be taken or not.
- Blood test: A blood test will measure the level of uric acid in your body.
- Joint aspiration: a small procedure which involves taking fluid out of the affected joint, using a needle and syringe.

Pacific and Māori communities
Pacific and Māori people have a demonstrated predisposition (or genetics) that result in higher uric acid levels in their bodies, and as a result are more affected by gout than other demographic group in New Zealand.
Statistics show that Pacific and Māori who are over the age of 20 are three times more likely to live with gout than other non-Pacific/non-Māori people, and that those aged between 20 and 44 are seven times more likely. They also experience a higher frequency of gout attacks accompanied with joint inflammation and severe disease, and have higher hospitalisation rates.
Furthermore, our traditional diets are rich in trigger foods like organ meats, seafood, and sugary beverages, and so that combined with genetic factors, contribute to elevated uric acid levels. That’s not to say that traditional foods are bad – in fact, they’re as likely to trigger attacks as any other types of food. It’s more about the combination of the food together with genetics, that requires Maori and Pacific to take more caution with their traditional foods than other ethnic groups.

When we effectively manage gout, we’re not just easing the pain of flare-ups; we’re improving our overall health too. By taking care of aspects like diet, genetics, and lifestyle choices, we can reduce how often and how badly gout hits.
For Māori and Pacific communities, where gout is more common, it’s about finding the right balance between traditional diet and modern treatments that work. When we get gout under control, it often means better management of other health issues like diabetes and heart disease, which are also common in our communities.
How can I prevent a gout attack?
The most effective way to reduce likelihood of getting an attack is by taking preventative medicines.
Statistics show that during the period of 2018-2019, about 26 percent of Pasifika males hospitalized for gout, were not receiving preventative gout medicine in the six months leading up to their hospitalisation, 21 percent had never received it at all, and 6 percent were on it six months prior, but did not continue after discharge.
It is vital that you speak to your GP or healthcare professional about options for preventative medicine, to avoid its severities.
Diet is also another way to help prevent flare-ups
A low purine diet is the best way to prevent frequent attacks. It centres around vegetables, wholegrains and fruit, and limits the consumption of red meats, alcohol and seafood.
It it is encouraged to incorporate more of the following into your diet:
- Water
- Lite or skim milk
- Vegetables
- Fruit (vitamin C rich)
- Low-fat dairy products
- Whole grains
- Nuts
It is encouraged to reduce the following in your diet:
- Seafood (including canned fish)
- Alcohol
- Sugary drinks (soda, energy drinks, satchet or sweetened juices)
- Red meats
- Yeast spreads (like marmite and vegemite)
Exercise and maintaining a healthy weight
Being overweight is also a contributing factor to having high levels of uric acid, so it is important to stay active and find time to exercise where you can.
Just take it steadily, one day at a time – as losing weight too fast can actually lead to an attack.

Pacific peoples health: gout data insights
Gout insights: impact on Māori
Eating & lifestyle advice for gout
Should people with gout avoid foods high in purine
To see a full list of our men’s health services, visit our service page here.



