Male health challenges
Male health in New Zealand faces significant challenges. Kiwi men are three times more likely than women to die by suicide. We’re 20% more likely to die from heart disease and twice as likely to be injured at work. Each year, 4000 men are diagnosed with prostate cancer, with around 700 fatalities. These stark figures highlight the importance of addressing male health issues head-on.
Many men are unaware that they have high blood pressure and are uncertain about their prostate health. They often engage in unsafe work practices that wear down their joints, drink too many nights a week, suffer from broken sleep, lack exercise, and consume food that increases their risk of diabetes. Many bottle up painful experiences, struggle with work stress, and may even face dark thoughts.

Many deaths among men are preventable with the right awareness and proactive measures. Early detection and treatment of conditions like heart disease, prostate cancer, and diabetes can significantly reduce mortality rates. By increasing awareness about these health issues and promoting regular check-ups, healthy lifestyles, and mental well-being, we can prevent many of the fatalities that affect men today. Understanding the risks and taking action is crucial for improving male health outcomes and ensuring longer, healthier lives.

In New Zealand, it is estimated that over 4000 men are diagnosed with prostate cancer annually, and that more than 600 of those cases result in death – it is the most common type of cancer affecting men in New Zealand, which makes it a key aspect of male health. It mostly affects men aged over 50 years old, but if it is detected in younger years then it becomes more likely to cause issues in the body.
What is prostate cancer?
The prostate is a small part of the male reproductive system. It is a gland that is located below the bladder, and it produces part of the fluid found present in semen.
When cells in the prostate start to grow abnormally, they can form into a lump or a tumour – which is known as prostate cancer.
What are the symptoms of prostate cancer?
There are generally no early warning signs of prostate cancer, but if you have any of these symptoms below, it is advised that you contact your doctor to get them checked out.
Symptoms include:
- Having difficulty passing urine
- Peeing more often than usual (especially at night)
- Experiencing pain when peeing (e.g. burning sensation)
- Having blood or semen present in your urine
- Stop and start flow in passing urine, or trouble doing either of those
- Unexplained weight loss
- Pain in the lower back or pelvic region
How is prostate cancer tested?
There are three different tests that can be done to check for prostate cancer:
- A blood test is performed to check the levels of a protein known as “Prostate Specific Antigen” or “PSA.” Every prostate, whether healthy or affected by cancer, produces PSA – but a high PSA level could indicate the presence of cancer.
- Moreover, your physician may conduct a prostate examination by inserting a gloved finger into your rectum to assess the gland’s condition without causing discomfort.
- A biopsy is a crucial procedure in which a small sample of potentially cancerous cells is taken for evaluation. After a prostate biopsy, it’s common for men to experience short-term instances of blood in their urine and, in some cases, observe blood in their semen.
Testicular cancer is the most common cancer in young men aged 18-39 (excluding non-melanoma skin cancer). In New Zealand, approximately 150 men are diagnosed with it each year, with 7-10 of those cases turning fatal. Although it most commonly affects males aged 15-39, it can occur in men of any age.
What is testicular cancer?
The testicles are the part of the male reproductive system that creates sperm. When the cells in the testicles start to grow abnormally into a lump or a tumour, it is known as testicular cancer.
What are the symptoms?
If you have one or more of these symptoms, it is important to get them checked out by your doctor:
- a swelling or lump presence in testicle
- changes to the shape or size of testicle
- sensation of heaviness or unevenness in scrotum
- discomfort in lower back or lower abdomen
- breast tissue swelling or becoming tender in your chest
In the early stages, testicular cancer may cause no signs except a painless lump. You can check abnormalities by: squeezing for lumps or bumps or feeling the tubes at the back for anything that feels unusual.

How is testicular cancer tested?
An ultrasound is used to scan for masses in the testicle. Your doctor can also run blood tests to look for specific tumour markers in the blood. Once these tests are positive, additional tests can be carried out such as a CT scan, MRI scan or an x-ray to see if the cancer has spread.

Every year, heart disease takes the lives of over 3,600 men in New Zealand. This illness hits Māori and Pacific men especially hard, with Māori men dying at more than twice the rate of non-Māori.
Why are men more prone to heart disease?
Men are generally more prone to heart disease than women due to a combination of biological, behavioural , and lifestyle factors.
One significant biological factor is the protective effect of estrogen, which helps maintain vascular health in women before menopause. Men, lacking this hormonal advantage, may develop heart disease at younger ages. Additionally, men often have higher levels of risk factors such as hypertension and cholesterol, which contribute to the development of heart disease.
Behavioural factors also play a crucial role. Men are more likely to engage in behaviours that increase their risk of heart disease, such as smoking, excessive alcohol consumption, and poor dietary choices. These habits contribute to the buildup of plaque in the arteries, leading to conditions like coronary artery disease. Furthermore, men are less likely to seek medical help or undergo regular health screenings, which means that risk factors and early signs of heart disease may go undetected and untreated for longer periods.
Lifestyle and occupational stress is another contributing factor. Men often work in high-stress environments or physically demanding jobs, which can increase their risk of heart disease. Chronic stress leads to elevated levels of cortisol and adrenaline, which can damage the cardiovascular system over time. Combined with a tendency toward less healthy coping mechanisms, such as alcohol use or overeating, these factors elevate the risk for men.
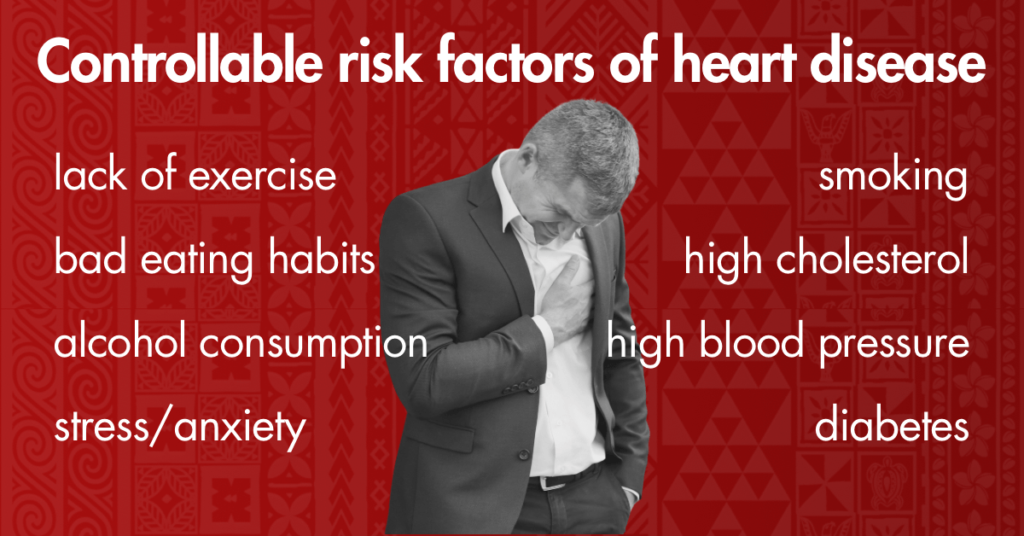
Māori and Pacific Men
The statistics for Māori and Pacific men in New Zealand highlight these issues starkly. Māori men have a mortality rate from heart disease that is more than twice that of non-Māori men. This disparity is due in part to socioeconomic factors, including limited access to healthcare, higher rates of smoking, and greater prevalence of conditions like diabetes and obesity, which are significant risk factors for heart disease. Pacific men also face higher rates of heart disease, driven by similar socioeconomic challenges and lifestyle factors, including dietary habits and lower rates of physical activity.
How do we address this?
Regular screenings, education on healthy lifestyles, and better access to healthcare services are essential steps in reducing the incidence of heart disease among men, particularly within the Māori and Pacific communities.
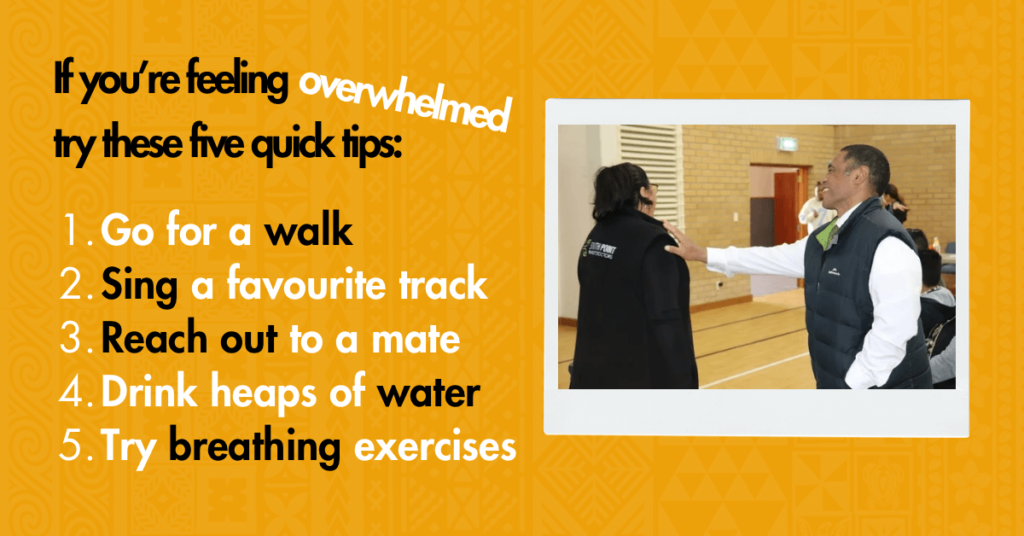
One main factor that affects male health in our country, is addressing mental health in our men. In recent years – largely thanks to the influence of social media – there has been a growing awareness regarding men’s mental health and the impact it has on our families and communities.
Due to masculine and cultural social norms, men – particularly Pasifika and Maori – are found to be more reluctant in expressing their feelings, viewing it as a sign of weakness.

A key role of emotions is to share our inner feelings with others, so when we bottle up our emotions inside, it often leads to withdrawing socially – resulting in less connection and decreased satisfaction with family and friends.
In addition to this, we are more likely to experience anxiety, depression, and other mental health issues when we are not able to talk about how we are feeling with others.
Suicide and Men
Males are more than twice as likely to die by suicide than females. In New Zealand, during the period of 2009 to 2022, the male suicide rate was significantly higher compared to females. In 2020 alone, men accounted for 72 percent of suicides.
Additionally, Maori and Pasifika had higher rates than any other ethnicities.

Promoting male health in New Zealand means making it easier and more acceptable for men to take care of themselves and seek the support they need. Remove the stigma of “weakness” that surrounds men seeking support, and normalise the topic by keeping the conversations open.
Let’s also celebrate male health achievements, ensuring that everyone feels supported in their journey towards a healthier life.
Check out our male health services and contact us to make an appointment for yourself, or a member of your whānau.

Gout: Important things to know
More info about testicular cancer
More info about prostate cancer
Umbrella – Breaking the silence: Men’s mental health in the workplace
Healthify: Men’s health topics
Tools for men’s health mental wellbeing
Mental wellbeing tools for family
One News “Men have it so easy” why do NZ men get minimal health support